Regulators have allowed thousands of nursing homes across America to flout federal staffing rules by going an entire day and night without a registered nurse on duty, a USA TODAY investigation has found.
Nearly all of them got away with it: Only 4{33c86113bcc32821f63c6372852a0f501e07fff55ce3ce61b15b246c5f8c531c} were cited by government inspectors. Even fewer were fined.
When other nursing home caregivers are added into the equation, one-third of U.S. facilities fell short of multiple benchmarks the federal government has created for nurse and aide staffing.
Low-income residents, disproportionately people of color, fare the worst. Their nursing homes report the lowest staffing levels, but data show they seldom get in trouble because of it.
A USA TODAY investigation has documented, for the first time, how rarely the federal government enforces decades-old staffing guidelines and rules for nursing homes.
Citations and penalties remained sparse even as regulators developed three ways to measure staffing. In the spring, they will propose a fourth approach.

Rich Pedroncelli/AP
Having enough nurses and aides is the strongest predictor of whether nursing home residents will thrive, researchers have found. When facilities are short-staffed, essential medical tasks are ignored. Doctor’s appointments are missed, call buttons go unanswered, diapers are not changed, showers are not given and wounds are not cleaned. Dementia can set in faster. People get sicker, and die, alone.
The desperation of residents and their relatives can be heard in emergency 911 calls.
“She is on the floor, and she can’t get anybody to get her off the floor,” one niece told a Louisiana dispatcher. “Can y’all do a wellness call or something? I don’t know what to do.”
On the other side of the state, a man unable to leave bed without assistance defecated on himself. He dialed 911.
“I called” for help, he told the dispatcher. “But nobody answered.”
In his State of the Union address this year, President Joe Biden promised sweeping nursing home reforms. But the government’s persistent failure to crack down on facilities that fall short of nursing home standards could render his plan ineffective.
USA TODAY compared millions of nursing home timesheets and thousands of inspection reports to the staffing numbers set down by federal rules and formulas. It found a staggering pattern of failure.
Charlene Harrington, one of the nation’s leading researchers on staffing levels and nursing home quality, said USA TODAY’s analysis probably underestimated how often facilities fell short because it used a conservative standard to measure care expected from nurses and aides.
“What you’re looking at is the bare minimum,” said Harrington, a professor emerita at the University of California, San Francisco. And federal regulators have “not even been enforcing the bare minimum.”

The problem existed long before COVID-19. Among facilities that did not have a registered nurse on duty eight hours a day as required by the federal Centers for Medicare & Medicaid Services (CMS), most failed to meet that standard in all three years before the coronavirus tore through nursing homes.
The pandemic did expose understaffing in nursing homes to many Americans. In its wake, former certified nurse assistant Tracey Pompey is floored that the public has not demanded better care for vulnerable elders.
“People get desensitized to things like this,” said Pompey, of Virginia. “If it happens to a child or a dog, people won’t shut up.”
Josh Morgan, USA TODAY
James Lovette-Black, a California nursing home inspector until 2020, offers a glimpse of how the problem persists. Lovette-Black said facilities often did not have enough nurses or aides to meet residents’ needs. Yet despite his best efforts, he said, “I don’t recall ever citing for staffing violations in any nursing home in my eight years.”
He echoed hundreds of inspectors surveyed for a study in 2013 as he described why. Staffing citations were not a priority set by department leaders, Lovette-Black said, and they were difficult to back up. He accused facilities of routinely beefing up staff during inspections, among other tactics documented by researchers, to avoid black marks on public ratings.
The American Health Care Association, the nation’s largest trade group for nursing homes, said in a news release this summer that 94{33c86113bcc32821f63c6372852a0f501e07fff55ce3ce61b15b246c5f8c531c} of the country’s facilities missed minimum staffing guidelines tougher than those used in USA TODAY’s analysis.
The organization said in an email that “the vast majority” of nursing homes provide inspectors with accurate information. That, senior vice president Holly Harmon said, is not the culprit.
“We firmly support transparency and accountability,” Harmon said, “and we must also foster an oversight system that recognizes good faith efforts and promotes improvement, not just penalties.”
Speaking of Biden’s plan, she added: “A new, federal staffing mandate without the available workforce and financial resources necessary to meet it would reinforce a punitive process that hasn’t been working for decades.”
Medicaid reimbursements, which pay for most nursing home stays, pays less than Medicare. The broader financial picture, however, is complicated.
Taxpayers spend nearly $90 billion each year on Medicaid and Medicare stays at nursing homes — many of them run by companies that report double-digit profit margins. Nursing homes also pay caregivers less than most other health care sectors.
Half of nursing staff — or more — turns over in a year, according to federal statistics on the industry.
Mike De Sisti, Milwaukee Journal Sentinel via USA TODAY NETWORK
Registered nurse Barbara Decelles made the best of it for 38 years at senior care centers in Wisconsin and Illinois. She quit last year.
She’s done working 25-hour shifts, knowing she might be making mistakes, then, exhausted, driving off the road on her way home.
She’s done choosing which call light to answer and which to ignore. She’s done asking for more help and being told it doesn’t fit the budget. She’s had it with owners appearing on a busy day to celebrate the staff’s heroic work with a goofy photo-op but not extending benefits to aides or awarding raises.
But she can’t escape from the anger – that people she cared for daily declined faster and died sooner because of inadequate staffing.
“Somehow, somebody is making money off of this, and it certainly isn’t the caregivers,” Decelles said. “I’m tired to my soul.”
Understaffing has been a problem throughout decades of nursing home reforms – one that Bill Halamandaris said leaders in Congress and at CMS have repeatedly sidestepped.
Halamandaris, a retired Capitol Hill staffer, worked on the Senate Committee on Aging as the nation wrote its first rules for nursing homes and granted broad authority to federal health officials to enforce them. Halamandaris said the 1967 Moss Amendments, among other things, were intended to lead to the creation of staffing minimums and a subsequent crackdown.
That didn’t happen.
“Like a lot of things, the congressional intent is lost in the bureaucracy,” Halamandaris said.
Federal regulators have since created multiple ways to measure whether a nursing home has enough staff.
Since the late 1980s, regulations have required facilities to have “sufficient nursing staff” to meet resident needs and to have a registered nurse in the building at least eight hours every day.
In 2001, a study commissioned by the Medicare regulator for Congress recommended minimum numbers of nurses and aides.
Then, beginning in 2011, CMS relied on the findings of a different study to determine how much to pay nursing homes for residents on Medicare. Reimbursements are calculated based on the level of staffing a typical nursing home provides for people with similar medical needs. It’s the formula CMS also deploys in its consumer-focused Nursing Home Care Compare tool.
That “expected” level of staffing, which USA TODAY used in its analysis, is almost always lower than the 2001 minimums.
Regulators have not used either the 2001 or 2011 benchmarks for enforcement. And USA TODAY found a chasm between facilities whose own filings with the federal government show they blew a third standard, the eight-hour rule, and those who get cited for it.
Nicholas Castle, a leading researcher on enforcement of nursing home standards from West Virginia University, said concentrated enforcement efforts also can have a significant effect. For instance, CMS and state inspection agencies focused for years on reducing the use of physical restraints.
Those restraints, he said, have “almost disappeared.”
Long-term care advocate Richard Mollot said that even without explicit numeric staffing requirements, the federal government’s qualitative approach combined with a wide array of available staffing benchmarks should provide plenty of leverage over short-staffing.
If inspectors “were empowered and interested, able or willing, to enforce this, I think the sufficient staffing requirement would be fine,” said Mollot, executive director of the Long Term Care Community Coalition. “But unfortunately, they’re unwilling or unable to do that.”
CMS declined multiple requests for an on-the-record interview about USA TODAY’s findings, staffing levels and oversight.
The results of timid enforcement play out daily in nursing homes across America.
Cindy Napolitan, 66, is an eyewitness to what short-staffing means at Cheyenne Medical Lodge in Mesquite, Texas, where she lives with her adult daughter. Both have multiple sclerosis, and Napolitan’s husband, who had been their caregiver, died in 2017.
Based on the 2001 federal study, the home should have enough aides to provide 2.8 hours of care per resident each day. The formula the government uses to pay the home Medicare money assumes it’s offering 2.4 hours. The real number for Cheyenne Medical Lodge? Each resident can expect 1.7 hours of aide care daily, according to its most recent reports to the government.
Napolitan described a struggle to get regular showers or help transferring into a wheelchair. She said her daughter developed a painful pressure ulcer because a doctor’s orders to turn her every two hours were not followed.

Cindy Napolitan
The administrator of Cheyenne Medical Lodge and its operating company, Foursquare Healthcare, did not respond to multiple requests for comment.
Since 2017, Texas nursing homes have reported the nation’s second-lowest staffing levels, USA TODAY found. Although more than 950 facilities reported fewer nurses or aides than expected by the Medicare formula, inspectors issued citations to just 16 of them – among the country’s lowest penalty rates.
A spokesperson for the Texas Department of Health and Human Services said inspectors “thoroughly investigate those concerns.” But assistant press officer Tiffany Young noted that the data collected by CMS is old before inspectors arrive, adding that they “are looking at staffing at that specific point in time.”
Napolitan has filed complaints, and when state inspectors made a repeat visit earlier this month, she said she quizzed them about whether her nursing home has had a record number of grievances.
“We don’t even come close,” she said. “That’s scary.”
She’s resigned to the fact that she’ll probably be fighting for good care for herself and her daughter as long as she can still communicate.
“I’m diplomatic; I try to be,” Napolitan said. “But there are times when you just have to say, ‘All right, enough is enough.’”
Residents of other nursing homes and their family members told USA TODAY they felt trapped. No matter where they went, they could not find adequate care. No matter who they told about staffing problems, they could not find someone to improve the situation.
In New York City, Claire Campbell encountered low staffing levels everywhere she took her mother, Grace E. Campbell.
USA TODAY’s analysis found that during her stays in two nursing homes between 2019 and 2022, the gap between actual staffing and CMS’ expected staffing ranked them in the state’s bottom third.
Even though Claire participated on the family council at one and filed numerous complaints with the state against both facilities, she said little ever changed.


Left: Grace Campbell filled out her 2020 absentee ballot during COVID lockdown at The Riverside Premier Rehabilitation and Healing Center in Manhattan. Right: In 2019, she dressed up for Halloween as “Grandma Noonie” – what her grandson called her.
Left: Grace Campbell filled out her 2020 absentee ballot during COVID lockdown at The Riverside Premier Rehabilitation and Healing Center in Manhattan. Right: In 2019, she dressed up for Halloween as “Grandma Noonie” – what her grandson called her.
SUBMITTED PHOTOS
In 2019, Grace entered The Riverside Premier Rehabilitation and Healing Center in Manhattan, a for-profit facility that overlooked the Hudson River.
She still was able to do the daily crossword in The New York Times and play along with “Jeopardy,” but she needed help standing up from the toilet. Instead, Claire said, nurses insisted her mother wear a diaper.
Delays in diaper changes, she claims, set off a chain reaction: Her mother avoided drinking water then suffered from dehydration and urinary tract infections.
In an email to USA TODAY, The Riverside administrator Jake Hartsein declined to discuss those allegations but denied that residents experience delays or omissions in care. He said that CMS recently gave the facility a five-star rating for some quality measures. He failed to mention that one-star ratings for health inspections and staffing pulled Riverside’s overall rating down to two stars.
When asked if he thought his staffing levels were adequate, Hartstein wrote: “In comparison with other skilled nursing facilities in our immediate proximity, The Riverside’s nurse aide (CNA) staffing levels are on the same level.”
After yet another fall, Grace moved from The Riverside to Amsterdam Nursing Home, a nonprofit, in the early summer of 2021. There, Grace routinely had to wait hours for help to use the bathroom, Claire said. She could not push her wheelchair over the marble threshold.
Because of the frequent delays, Claire said, she hired an aide to visit her mother at the nursing home. Even that did not guarantee timely care.
On Claire’s birthday in January, Grace called saying she had to have a bowel movement but no one had helped. Claire and a friend abandoned their lunch to rush over.


While living at New York’s Amsterdam Nursing Home, Grace Campbell fell on Jan. 4 after, her daughter says, she tried to move herself in her wheelchair when no one answered her call light. These photos, from Jan. 10 and Jan. 11, show the bruises that developed.
While living at New York’s Amsterdam Nursing Home, Grace Campbell fell on Jan. 4 after, her daughter says, she tried to move herself in her wheelchair when no one answered her call light. These photos, from Jan. 10 and Jan. 11, show the bruises that developed.
SUBMITTED PHOTOS
Within an hour, Grace, 98, was dead. Her death certificate read “natural causes.”
In a statement to USA TODAY, a spokesperson for the management company with which Amsterdam Nursing Home contracts, Centers Health Care, said “safety and care” are the top priority.
Corporate communications director Jeff Jacomowitz said in a statement that the facility meets all state staffing requirements. Yet, Amsterdam Nursing Home was cited for insufficient staffing by the department’s inspectors in February, just weeks after Grace’s death.
Government penalties for insufficient staffing are rare in the state of New York. Of the facilities reporting levels below those expected by the Medicare formula, only 3{33c86113bcc32821f63c6372852a0f501e07fff55ce3ce61b15b246c5f8c531c} were cited for it.
The inspectors who visited Amsterdam showed how it could be done. They compared daily staffing reports with the facility’s assessment of complete staffing, finding enough caregivers on just four days in January 2022.
One nursing assistant interviewed by inspectors called the situation “a nightmare.” She said she was embarrassed to answer the phone and talk to family members who wondered why their relative had not been taken out of bed that day. “I can’t take 18 people out of bed when there are only two staff,” she said. “It’s impossible.”
Inspectors also had issued a citation for insufficient staffing to The Riverside in May 2019, when Grace was a resident. Neither that citation nor the one for Amsterdam ended in fines.
“Ensuring all nursing home residents receive proper care is a priority of the New York State Department of Health,” said Deputy Director of Communications Jeffrey Hammond. He also noted that inspections “are conducted in accordance with federal regulations.”
A new state law that took effect in April requires nursing homes to spend at least 40{33c86113bcc32821f63c6372852a0f501e07fff55ce3ce61b15b246c5f8c531c} of their revenue on staff that provides face-to-face care.
“I reported it to everyone,” Claire Campbell said of the understaffing and poor care. “From the nursing station to the medical director to the wound care director to the ombudsmen to the State of New York Department of Health. … Nobody took action.”
Part of the president’s plan to address lax enforcement of nursing home rules is to pay states to hire more nursing home inspectors and boost their pay.
Inspectors, who often are registered nurses, can find better wages and less out-of-town travel in the private sector. Federal funding for nursing home enforcement has not changed since 2014: about $397 million a year. Biden wants to increase that by 25{33c86113bcc32821f63c6372852a0f501e07fff55ce3ce61b15b246c5f8c531c}, matching inflation over the past seven years.
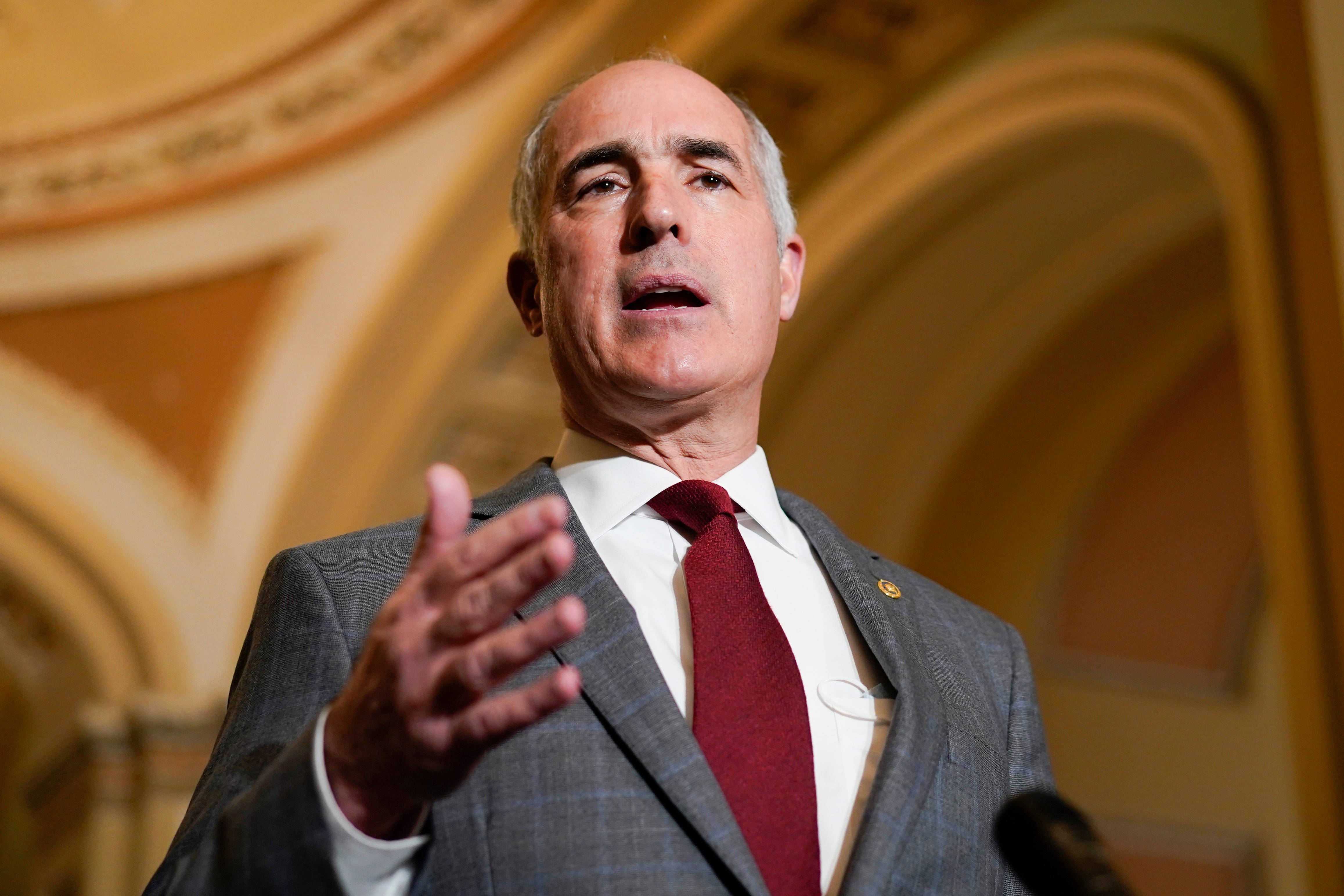
Carolyn Kaster, AP
Sen. Bob Casey, a Democrat from Pennsylvania who has pushed for tougher enforcement on the worst nursing homes, supports the funding increase.
“I’ve been advocating … for years now, for not just transparency and accountability with regard to nursing homes themselves,” he said, “but also the resources that will bring about that transparency, accountability and better performance.”
Casey notes that a January report from the Inspector General for the Department of Health and Human Services found inspection agencies understaffed. A quarter of states routinely miss a federal deadline to inspect a home within 10 days of receiving a safety complaint.
In letters to state officials this fall, Casey said about a third of nursing homes are overdue for standard annual inspections. Some states are doing far worse than others.
Inspectors also have reported frustrations with the job. The 2013 survey of hundreds of nursing home inspectors in 10 states found widespread pressure from industry and elected officials to change inspection results.

Brian Myszkowski, USA TODAY NETWORK
“We are being crushed by political influence of the nursing home groups,” one inspector wrote.
Some inspectors said they would recommend fines or even stiffer penalties only to have their bosses “downcode” their reports. A reversal that “throws out things you work so hard on can be discouraging,” another inspector wrote.
Dean Lerner, an attorney who oversaw regulatory enforcement in Iowa for nearly a decade, said he once expanded the state’s team of nursing home inspectors because they “were so understaffed.” But, he said, the incoming governor cut those positions before anyone could start.
Sometimes CMS’ own guidance has created confusion.
The federal manual given to states to train their inspectors for years told them they should not investigate staffing levels unless the inspector had first found that care standards were not met. It’s like handing out speeding tickets only to drivers who crash.
A year after regulations changed in 2016, that guidance was updated, allowing inspectors to look into staff at any time and without needing to link low staffing to poor care. But the rarity of citations, coupled with observations of inspectors, suggests some still believe they need examples of care violations.
That’s not the only barrier confronted by inspectors. Nurses told USA TODAY they have been threatened with termination if they speak honestly to inspectors. Others feared they could be held personally responsible for poor care caused by understaffing beyond their control.
Nurses also confessed they had given falsified staffing data to inspectors during visits or called in extra workers on days they learned inspectors would be coming. Academic research has found staffing spikes around inspection days.
Lovette-Black, the retired California state inspector, recalled seeing the same staffing-related problems – “frequent falls or pressure injuries or infections,” he said – year after year at the same facilities. By submitting paperwork that testifies they had retrained their staff members or had adjusted staffing schedules, he said, the nursing homes would be deemed back in compliance.
“A year later when you went back, they would have slipped back into their bad practices,” he said. “There still wasn’t enough CNAs. Wasn’t enough licensed nurses.
“Nothing really changes. The culture doesn’t change.”
After David Jones, 71, had a stroke, he was sent to a Virginia nursing home for a few weeks of physical therapy to regain use of his leg. He and his wife chose Glenburnie Rehab and Nursing Care Center, a facility near their predominantly Black neighborhood in Richmond.
The proximity made it easier for Jones’ elderly wife and daughter – a nurse’s aide – to spend time with him daily. After retiring from his job as a hospital janitor, Jones had loved to travel and especially enjoyed fishing trips in the rural countryside where he grew up. Friends and other family members visited him in the nursing home.
Low staffing is particularly acute at nursing homes that serve a high proportion of nonwhite residents. That includes many facilities in Virginia like Glenburnie Rehab, where about half the residents are Black.
At Virginia facilities with more residents of color, only 7{33c86113bcc32821f63c6372852a0f501e07fff55ce3ce61b15b246c5f8c531c} met the staffing levels they were expected to employ based on the Medicare payment formula. Among all other nursing homes in Virginia, 30{33c86113bcc32821f63c6372852a0f501e07fff55ce3ce61b15b246c5f8c531c} hit that mark.
Yet only eight staffing citations were issued to any nursing home in Virginia last year. Three of them went to predominantly Black homes.
Kimberly Beazley, director of the Virginia office that oversees nursing home licenses and inspections, said the division has historically had more turnover than other teams. She said 30{33c86113bcc32821f63c6372852a0f501e07fff55ce3ce61b15b246c5f8c531c} of inspector positions are now vacant.
But Beazley said she does not think vacancies have affected the quality of inspections, only the quantity inspectors can complete. Asked whether the state was issuing enough citations for staffing violations, she said, “We have followed all CMS’ guidance.”
Researchers have connected the disparity in staffing to higher for-profit ownership of nursing homes in Black communities and the fact that more Black residents pay for their stays with Medicaid, which reimburses nursing homes at a lower rate. Some are too young for Medicare; others end up there beyond the usual 21 days covered by that benefit.
Tetyana Shippee, associate director of research at the Center for Healthy Aging and Innovation at the University of Minnesota, said the racial disparities in COVID-19 deaths brought attention to a little-discussed niche of nursing home research: the health and quality-of-life consequences of structural racism in policies and practices.
“Nursing homes are the most racially segregated aspect of health care,” she said. People who go to a facility where fewer residents are white will have different outcomes, she said. “Regardless of your health profile, you’re going to have worse quality of care.”
Tracey Pompey, a nurse’s aide in Virginia for 30 years, saw the disparities while working as an on-call agency nurse in dozens of facilities.
Josh Morgan, USA TODAY
“No one is being held accountable for what is happening in these facilities,” said Pompey, a co-founder and vice president of the advocacy organization Justice and Change for Victims of Nursing Facilities. “I saw firsthand how patients are treated, how horrible the staffing levels are.”
David Jones is Pompey’s father. She experienced the system from a new vantage point when writing a complaint about his care at Glenburnie, in which she described how she believed nurses and aides had failed to adequately address serious symptoms in the hours leading up to his death and did not notify family of his condition as required.
The administrator at Glenburnie did not return multiple requests for comment.
USA TODAY found that in every quarter since 2017, Glenburnie timecards reported fewer nurses and aides on hand than expected based on the federal reimbursement formula. At the time of Jones’ 2015 stay, federal regulators used a previous system to track staffing levels. That self-reported data shows Glenburnie fell short on aides, who provide the bulk of care, and registered nurses, who are trained to assess resident medical conditions.
Since 2015, the nursing home has never been cited for short staffing.
On his fifth day at the facility, Jones complained of stomach pain. His belly was swollen. For hours he vomited stool, according to a 74-page state report. A nurse documented each of his complaints. The facility also noted he had not had a bowel movement in four days.
An X-ray done at the facility showed Jones’ intestines were twisted, but no change in care was ordered beyond giving him giving him oral medications for stomach acid and constipation, along with a probiotic, according to the state report. No one did an abdominal exam.
Ten hours later, at about 2:30 a.m., a registered nurse on the next shift asked an aide to stay with Jones while she called 911, then his family. When she returned with the EMTs, the state report says, Jones was alone, face down on the floor.
His heart stopped before he could be carried into the ambulance.
An inspector issued citations against Glenburnie related to Jones’ death: failing to notify family about a change in condition, failing to maintain a resident’s well-being, and not keeping complete medical records.
A state review of time-stamped charting notes shows a manager at the facility amended Jones’ record days after his death to describe check-ins and care – some of which the review indicates the facility was unable to back up with additional documentation or that did not match staff interviews.
Reflecting recently, Pompey remains frustrated that the facility was not fined for her father’s death. And she is left to wonder whether a lack of training or understaffing played a role.
“We feel that had they gotten him to the hospital sooner, things could’ve been different,” she said. “Somebody should’ve said, ‘Something’s wrong.’”
When Biden was vice president, the Obama administration had a shot in 2016 at making the rules for nursing homes more explicit. Academics and advocates were calling for numeric staffing minimums to be written into new federal rules — and for those minimums to be enforced.
The administration chose a different path.
“We agree that sufficient staffing is necessary,” CMS wrote in the Federal Register. “However, we do not agree that we should establish minimum staffing ratios at this time.”
Instead, the agency decided, nursing home managers would have to conduct a “facility assessment” listing how many workers the facility would have on hand, a number they’re supposed to develop based on the medical conditions of residents.

KELLY MARSH/FOR THE TIMES HERALD
Little changed. USA TODAY found staffing levels at nursing homes have actually decreased 9.4{33c86113bcc32821f63c6372852a0f501e07fff55ce3ce61b15b246c5f8c531c} since 2017, when the assessments were first required. And penalties for understaffing remain rare.
Now under order from Biden as president, CMS plans to propose explicit minimums next year for each nursing role, which it says should push facilities to improve. It could be years more before new rules take effect or are enforced.
“Having something that’s more objective and numerical … would be useful for increased enforcement relative to the existing, more qualitative standard,” said Hannah Garden-Monheit, special assistant to the president from the National Economic Council.
But the data also shows putting numbers on the books is no guarantee they will be enforced.
In the vacuum of federal staffing minimums, 35 states stepped up to set their own, with varied results. Few wrote rules for both nurses and aides. None require the staffing minimums recommended by federal regulators in 2001.
Oregon, for instance, requires at least 2.46 hours of daily care per resident from nurses and aides.
The northwestern state has the lowest percentage of facilities reporting low staffing and among the highest rates of enforcement, USA TODAY found. Last year, fewer than half of Oregon nursing homes reported less staff than expected in the federal payment formula. Inspectors issued citations to 44{33c86113bcc32821f63c6372852a0f501e07fff55ce3ce61b15b246c5f8c531c} of those that did – more than six times higher than the U.S. average.
“Staffing is something we care deeply about in Oregon as inadequate staff is often the cause of safety and quality of care issues,” Department of Human Services communications manager Elisa Williams wrote in an email.

FILE/STATESMAN JOURNAL
Louisiana also wrote its own staffing rules, but more nursing homes there fail to meet expectations, suggesting that state rules are not a cure-all if they are not enforced. It requires facilities to provide each resident at least 2.35 hours of care each day from nurses, aides and, sometimes, ward clerks.
Last year, only 1 in 10 Louisiana nursing homes had as much staffing as CMS expected based on the reimbursement formula. The state also has the nation’s lowest levels of daily RN care in the five years reviewed: 16 minutes per resident compared with 38 minutes nationwide, a total that counts nurses working in administrative jobs.
Yet only five facilities were cited for short-staffing. Zero were cited for not having a registered nurse on duty at least eight hours a day even though 78{33c86113bcc32821f63c6372852a0f501e07fff55ce3ce61b15b246c5f8c531c} of Louisiana’s nursing homes fell short at least once.
The Louisiana Department of Health said in an emailed statement that every inspection includes a review of staff levels. Inspectors also review staffing when investigating specific cases of poor care. Citations are issued, the department email said, “if there is sufficient evidence.”
Jacinda Gaston often smelled urine when she stepped off the elevator to start her shift on the fourth floor of Alden Lakeland, an Uptown Chicago nursing home.
Residents who could speak told her they had been sitting in soiled diapers for eight or more hours. Urine and stool ran up people’s backs to their necks and the entire bed had to be changed.
She said it was a blessing when another aide shared the load.
“You have to make the decision: ‘What room can I get to first?’ Knowing in the back of your head there are people who are going to have to wait even longer,” said Gaston, an aide at the facility for five months this year. “Then you have the people who don’t understand. They’re constantly on their call light. By the time you get to them, they’re in tears.”
Two inspection reports from this year document the understaffing at Alden Lakeland. In February, the director of nursing told inspectors that the fourth floor was supposed to have at least five certified nursing assistants to care for the 74 residents – not two.
The nursing home is one of six facilities named in a class action lawsuit recently filed against The Alden Network, among the largest nursing home operators in Chicago. Gaston has volunteered as a witness for the plaintiffs.
In a statement to the Chicago Tribune, Alden officials said they do not comment on pending litigation but wrote that the company “vigorously denies any and all allegations of wrongdoing.”

Mustafa Hussain for USA TODAY
Alden’s vice president of policy and public relations, Janine Schoen, declined to answer questions from USA TODAY, including whether the owners believe staffing has been adequate at Lakeland. Instead, she focused on the company’s recruiting efforts, which she described as expansive, and called for action from the state and national capitals.
“We need our leaders in Springfield and Washington to focus on actionable solutions to attract more caregivers to the industry rather than punitive acts that fail to solve the underlying labor shortage,” Schoen wrote.
Complaints about Alden Lakeland prompted more frequent inspections than the federal minimum of once every year and three months. Since 2012, inspectors have shown up 28 times and issued 90 citations.
Their reports documented abuse, broken bones, head wounds, medication errors, pressure ulcers that threatened lives, residents with dementia wandering unsupervised, improper use of physical restraints, cloudy catheter tubes, mice infestations and staff members providing care beyond the scope of their licenses.
Residents went months without leaving their beds, weeks without showers and hours without a diaper change.
In the 11-year span covered by those reports, Alden Lakeland was fined only once. In 2016, the facility paid $1,991 for failing to report and investigate abuse or neglect. Three years later, inspectors issued the same citation but no fine when the facility did not investigate how a resident’s femur had snapped.
Until this year, none of Alden Lakeland’s citations were for short-staffing.
Overall, Illinois nursing homes had the lowest staffing in the nation across the five years reviewed by USA TODAY. Last year, 91{33c86113bcc32821f63c6372852a0f501e07fff55ce3ce61b15b246c5f8c531c} of nursing homes missed the mark set in the Medicare formula.
The state also has been more likely than most to issue staffing citations against nursing homes, USA TODAY’s analysis found – which still meant inspectors wrote up only 14{33c86113bcc32821f63c6372852a0f501e07fff55ce3ce61b15b246c5f8c531c} of facilities whose timesheets showed they had missed the expected staffing level.
Given the increasing focus from state and federal officials, the Illinois Department of Public Health “anticipates increased inquiry into staffing” during inspections, said spokesperson Michael Claffey.
Last year, Alden Lakeland had fewer nurses and aides on hand than most nursing homes in the state: 2.7 hours of care per resident each day, a ratio similar to figures the facility reported in previous years.
That’s 1.1 hours less care than the staffing the nursing home should have based on the Medicare reimbursement formula and 1.4 hours under what Medicare and Medicaid’s 2001 report found essential to avoid medical errors.
The most recent staffing figures for Alden Lakeland are even lower.
Gaston, the former Alden Lakeland aide, said she once found a resident with dementia locked inside a shower room. He had been there at least three hours. Twice, Gaston remembers, a resident left the building unnoticed.
Mary Anne Miller, a retired physical therapist who worked at Alden Lakeland in 2018 and 2019, described the daily struggle to find an aide to help her move residents from bed into a wheelchair so they could attend therapy.
Like Gaston, Miller has volunteered to testify against The Alden Network in the pending lawsuit.
“I couldn’t work there after a while because it was too heartbreaking,” she said. “It’s not because the staff isn’t trying. It’s just because there’s not enough staffing.”
Illinois lawmakers recently enacted reforms aimed at boosting staff and quality. The state has raised its staffing minimums and changed Medicaid payments to incentivize increasing staff and wages.
At Alden Lakeland, five inspection reports from this year noted the same kinds of poor care documented in dozens of earlier visits. But, for the first time, regulators issued three citations for insufficient staffing.
In May, a state inspector found two residents alone in the dining room, one eating with their fingers. Both had significant cognitive impairments and difficulty swallowing. Under medical order, they were to be monitored to ensure they not only ate enough but didn’t inhale food into their lungs or choke to death.
An aide informed the inspector that “there’s not enough staff” to watch or to help them eat.
The inspector deemed it an isolated event and issued a citation that would not trigger a fine: “Minimal harm.”
Contributing: Maria Clark and Claire Withycombe, USA TODAY Network; Lauren Formosa, Jared Sweet and Audrey Whitaker, Grand Valley State University.
This report received support from the Economic Hardship Reporting Project.
Jayme Fraser and Nick Penzenstadler are reporters on the USA TODAY investigations team. Contact Jayme at [email protected], @jaymekfraser on Twitter and Facebook, or on Signal and WhatsApp at (541) 362-1393. Contact Nick at [email protected] or @npenzenstadler, or on Signal at (720) 507-5273. Jeff Kelly Lowenstein is the Padnos/Sarosik Endowed Professor of Civil Discourse at Grand Valley State University.




More Stories
State retires its nursing home order — and 2 counties immediately reinstate it
‘Access Crisis Unfolding’: Nursing Home Operators, Advocates Warn of Dire Effects from Biden’s Order on Staffing
Nursing home staffers aren’t getting a living wage, and needed beds are empty. The industry wants taxpayers to help | Local News